Stroke unit
Ideally, people who have had a stroke are admitted to a "stroke unit", a ward or dedicated area in hospital staffed by nurses and therapists with experience in stroke. It has been shown that people admitted to a stroke unit have a higher chance of surviving than those admitted elsewhere in hospital, even if they are being cared for by doctors with experience in stroke.
When an acute stroke is suspected by history and physical examination, the goal of early assessment is to determine the cause. Treatment varies according to the underlying cause of the stroke, thromboembolic (ischemic) or hemorrhagic. A non-contrast head CT scan can rapidly identify a hemorrhagic stroke by imaging bleeding in or around the brain. If no bleeding is seen, a presumptive diagnosis of ischemic stroke is made.
Treatment of ischemic stroke
Ischemic stroke is caused by a thrombus (blood clot) occluding blood flow to an artery supplying the brain. Definitive therapy is aimed at removing the blockage by breaking the clot, thrombolysis, or by removing it mechanically, thrombectomy. The more rapidly bloodflow is restored to the brain, the fewer brain cells die.
Other medical therapies are aimed at minimizing clot enlargement or preventing new clots from forming. To this end, treatment with medications such as aspirin, clopidogrel and dipyridamole may be given to prevent platelets from aggregating.
In addition to definitive therapies, management of acute stroke includes control of blood sugars, ensuring the patient has adequate oxygenation and adequate intravenous fluids. Patients may be positioned with their heads flat on the stretcher, rather than sitting up, to increase blood flow to the brain. It is common for the blood pressure to be elevated immediately following a stroke. Although high blood pressure may cause some strokes, hypertension during acute stroke is desirable to allow adequate blood flow to the brain.
Thrombolysis
In increasing numbers of primary stroke centers, pharmacologic thrombolysis ("clot busting") with the drug tissue plasminogen activator (tPA), is used to dissolve the clot and unblock the artery. However, the use of tPA in acute stroke is controversial. On one hand, it is endorsed by the American Heart Association and the American Academy of Neurology as the recommended treatment for acute stroke within three hours of onset of symptoms as long as there are not other contraindications (such as abnormal lab values, high blood pressure, or recent surgery). This position for tPA is based upon the findings of two studies by one group of investigators which showed that tPA improves the chances for a good neurological outcome. When administered within the first three hours, 39% of all patients who were treated with tPA had a good outcome at three months, only 26% of placebo controlled patients had a good functional outcome. A recent study using alteplase for thrombolysis in ischemic stroke suggests clinical benefit with administration 3 to 4.5 hours after stroke onset. However, in the NINDS trial 6.4% of patients with large strokes developed substantial brain hemorrhage as a complication from being given tPA. tPA is often misconstrued as a "magic bullet" and it is important for patients to be aware that despite the study that supports its use, some of the data were flawed and the safety and efficacy of tPA is controversial. A recent study found the mortality to be higher among patients receiving tPA versus those who did not. Additionally, it is the position of the American Academy of Emergency Medicine that objective evidence regarding the efficacy, safety, and applicability of tPA for acute ischemic stroke is insufficient to warrant its classification as standard of care.
Mechanical thrombectomy
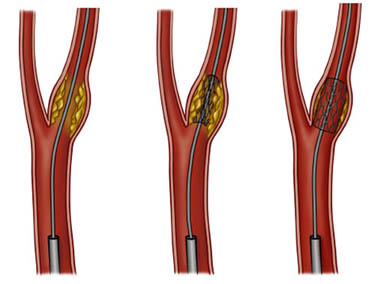
Another intervention for acute ischemic stroke is removal of the offending thrombus directly. This is accomplished by inserting a catheter into the femoral artery, directing it into the cerebral circulation, and deploying a corkscrew-like device to ensnare the clot, which is then withdrawn from the body. Mechanical embolectomy devices have been demonstrated effective at restoring blood flow in patients who were unable to receive thrombolytic drugs or for whom the drugs were ineffective, though no differences have been found between newer and older versions of the devices. The devices have only been tested on patients treated with mechanical clot embolectomy within eight hours of the onset of symptoms.
Therapeutic hypothermia
Most of the data concerning therapeutic hypothermia’s effectiveness in treating ischemic stroke is limited to animal studies. These studies have focused primarily on ischemic as opposed to hemorrhagic stroke, as hypothermia has been associated with a lower clotting threshold. In these animal studies investigating the effect of temperature decline following ischemic stroke, hypothermia has been shown to be an effective all purpose neuroprotectant. This promising data has lead to the initiation of a variety of human studies. Unfortunately, at the time of this article’s publishing, this research have yet to return results. However, in terms of feasibility, the use of hypothermia to control intracranial pressure (ICP) after an ischemic stroke was found to be both safe and practical. The device used in this study was called the Arctic Sun
Secondary prevention of ischemic stroke
Anticoagulation can prevent recurrent stroke. Among patients with nonvalvular atrial fibrillation, anticoagulation can reduce stroke by 60% while antiplatelet agents can reduce stroke by 20%.. However, a recent meta-analysis suggests harm from anti-coagulation started early after an embolic stroke. Stroke prevention treatment for atrial fibrillation is determined according to the CHADS/CHADS2 system.
If studies show carotid stenosis, and the patient has residual function in the affected side, carotid endarterectomy (surgical removal of the stenosis) may decrease the risk of recurrence if performed rapidly after stroke.
Treatment of hemorrhagic stroke
Patients with intracerebral hemorrhage require neurosurgical evaluation to detect and treat the cause of the bleeding, although many may not need surgery. Anticoagulants and antithrombotics, key in treating ischemic stroke, can make bleeding worse and cannot be used in intracerebral hemorrhage. Patients are monitored and their blood pressure, blood sugar, and oxygenation are kept at optimum levels.
Care and rehabilitation
Stroke rehabilitation is the process by which patients with disabling strokes undergo treatment to help them return to normal life as much as possible by regaining and relearning the skills of everyday living. It also aims to help the survivor understand and adapt to difficulties, prevent secondary complications and educate family members to play a supporting role.
A rehabilitation team is usually multidisciplinary as it involves staff with different skills working together to help the patient. These include nursing staff, physiotherapy, occupational therapy, speech and language therapy, and usually a physician trained in rehabilitation medicine. Some teams may also include psychologists, social workers, and pharmacists since at least one third of the patients manifest post stroke depression. Validated instruments such as the Barthel scale may be used to assess the likelihood of a stroke patient being able to manage at home with or without support subsequent to discharge from hospital.
Good nursing care is fundamental in maintaining skin care, feeding, hydration, positioning, and monitoring vital signs such as temperature, pulse, and blood pressure. Stroke rehabilitation begins almost immediately.
For most stroke patients, physical therapy (PT) and occupational therapy (OT) are the cornerstones of the rehabilitation process, but in many countries Neurocognitive Rehabilitation is used, too. Often, assistive technology such as a wheelchair, walkers, canes, and orthosis may be beneficial. PT and OT have overlapping areas of working but their main attention fields are; PT involves re-learning functions as transferring, walking and other gross motor functions. OT focusses on exercises and training to help relearn everyday activities known as the Activities of daily living (ADLs) such as eating, drinking, dressing, bathing, cooking, reading and writing, and toileting. Speech and language therapy is appropriate for patients with problems understanding speech or written words, problems forming speech and problems with swallowing.
Patients may have particular problems, such as complete or partial inability to swallow, which can cause swallowed material to pass into the lungs and cause aspiration pneumonia. The condition may improve with time, but in the interim, a nasogastric tube may be inserted, enabling liquid food to be given directly into the stomach. If swallowing is still unsafe after a week, then a percutaneous endoscopic gastrostomy (PEG) tube is passed and this can remain indefinitely.
Stroke rehabilitation should be started as immediately as possible and can last anywhere from a few days to over a year. Most return of function is seen in the first few days and weeks, and then improvement falls off with the "window" considered officially by U.S. state rehabilitation units and others to be closed after six months, with little chance of further improvement. However, patients have been known to continue to improve for years, regaining and strengthening abilities like writing, walking, running, and talking. Daily rehabilitation exercises should continue to be part of the stroke patient's routine. Complete recovery is unusual but not impossible and most patients will improve to some extent : a correct diet and exercise are known to help the brain to self-recover.